HGH vs Peptides: What’s the Difference?
Have you tested this hormone?
When we think of “hormones,” most women think of estrogen, progesterone, or maybe testosterone. But there’s another hormone that quietly shapes your vitality long before perimenopause or menopause symptoms begin. IGF-1, the growth hormone metabolite, is almost never tested, yet many women experience symptoms associated with its decline.
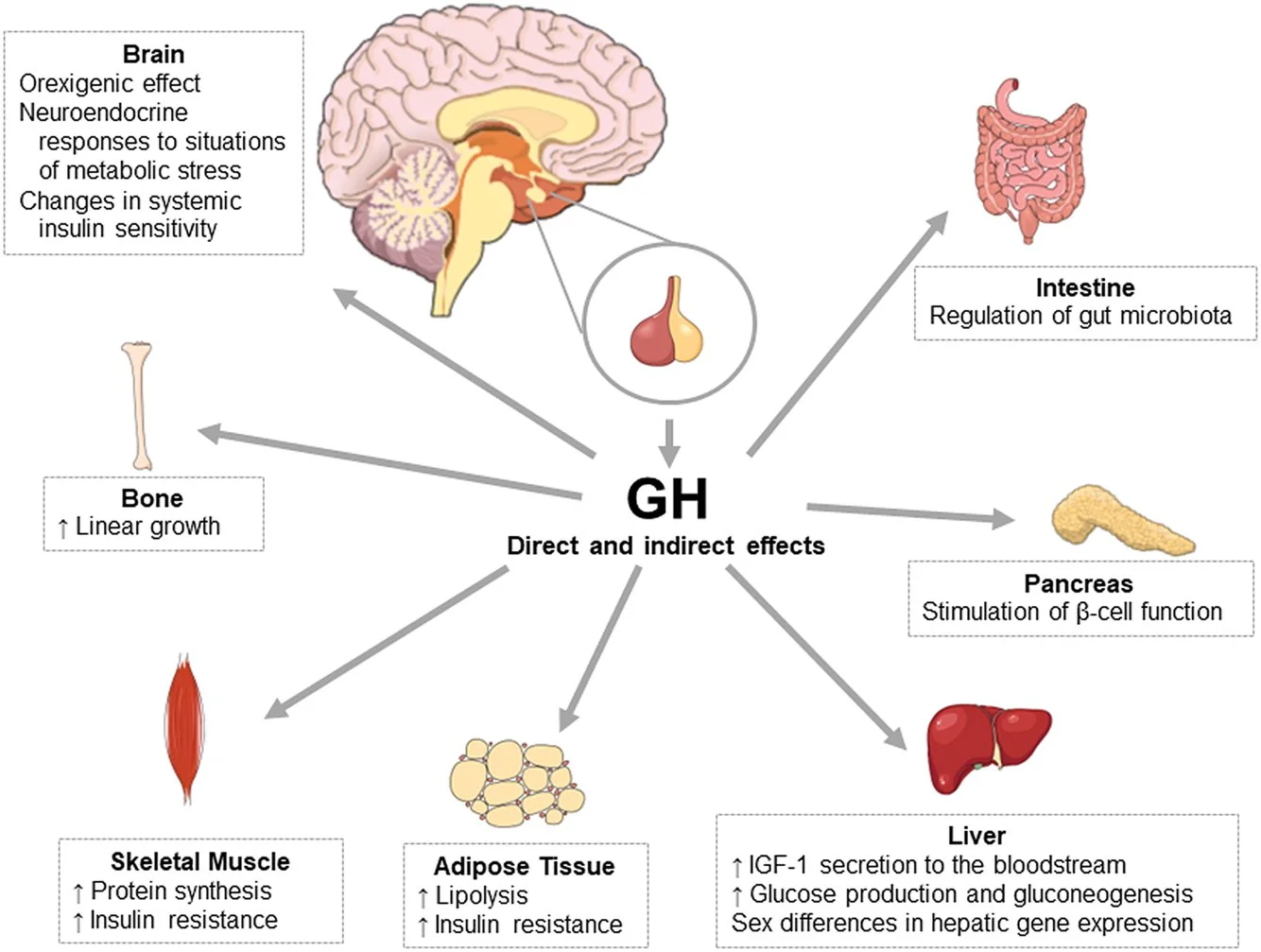
Why growth hormone, GH, matters: it’s not just for growth
Fuels muscle repair & strength
Stimulates collagen production
Supports deep sleep & brain health
Enhances fat metabolism & energy
The catch? GH peaks in your 20s and steadily declines each decade. By perimenopause, low GH can look like: stubborn belly fat, slower recovery, thinning skin, and fatigue.
When most people hear “growth hormone,” they think of the synthetic form, HGH, Human Growth Hormone. But, that’s not what I’m talking about here.
HGH vs Peptides: What’s the Difference?
HGH (Human Growth Hormone): Prescription hormone replacement. It can raise GH levels but comes with risks—fluid retention, insulin resistance, elevated blood sugar and accelerated aging if not monitored carefully. For true GH deficiency, this needs to be closely monitored.
Peptides (like CJC-1295, Ipamorelin, Sermorelin, and Tesamorelin): These signal your own pituitary to release GH in a more natural rhythm. Think of it as nudging your body to produce its own growth hormone rather than flooding the system. For most women, peptides are a gentler, safer option when clinically indicated.
Natural ways to support GH right now:
Deep sleep: GH pulses during early-night deep sleep—bedtime before 11pm is golden.
Strength training: Lifting weights stimulates GH release, especially in the morning hours.
Intermittent fasting: Extends GH pulses and improves metabolism.
Arginine (taken away from food, before bed): An amino acid that can enhance GH secretion by lowering its natural “off switch.”
Cold exposure: Cold plunges or even a brisk cold shower can spike GH naturally.
Declining growth hormone is one of the earliest hormone shifts women experience. Supporting GH can also boost your testosterone, and contribute to more muscle, better sleep, a faster metabolism, and prevent premature aging in the decades ahead.
How to work with your healthcare provider:
Most likely, your PCP is not familiar with how to manage GH levels that are not clinically low when target IGF-1 levels should be between 150-215 ng/dL.
Research healthcare providers using A4M or Seeds Institute directory to find someone who can properly do a full workup and introduce peptides if necessary, in a safe way.
Peptides should never be prescribed as the only solution. They work the best when prescribed along with proper nutrition, sleep hygiene, exercise and when the whole person is addressed.
Red flag: you’re being prescribed a research peptide. Ask your healthcare provider what kind of a pharmacy they are using. There are many influencers and health coaches promoting peptides. They do not have the medical background to tell you what’s appropriate or not, and do not see through the same lens as medical professionals trained in peptide therapy. Experience and quality assurance matters, and that applies to everything from supplements to HRT and peptides.
GH and cancer?
Growth hormone does not cause cancer. However, if you have a history of cancer or are actively being treated for cancer, this is not the first place to start.
Cancer is more complex than just one hormone or one factor leading to its development. More often than not, it has more to do with inflammation and immune system regulation. Obesity, environmental toxin exposure, alcohol consumption and declining hormone levels, which actually regulate our immune system, are some of the bigger factors that contribute to poor cell function.